1. Introduction
1. The right to protection of health is enshrined in
Article 11 of the revised European Social Charter, which is worth
recalling: “With a view to ensuring the effective exercise of the
right to protection of health, the Parties undertake, either directly
or in co-operation with public or private organisations, to take
appropriate measures designed
inter alia:
to remove as far as possible the causes of ill-health; to provide
advisory and educational facilities for the promotion of health
and the encouragement of individual responsibility in matters of
health; to prevent as far as possible epidemic, endemic and other
diseases, as well as accidents”.

2. Following
Recommendation
1626 (2003) of the Council of Europe’s Parliamentary Assembly
on the reform of health care systems in Europe: reconciling equity,
quality and efficiency, the Committee of Ministers declared in 2004
that “the Council of Europe will continue to play an important role
in assisting member states to incorporate the ethical, social and
human rights dimension in health policies and in reforms of their
health care systems. Continuing attention will be paid to access
for the vulnerable and in finding a new balance between curative,
preventive and promotive health care”.

3. In the Oslo Declaration on Health, Dignity and Human Rights,
the European Health Ministers meeting in Oslo on 12 and 13 June
2003 called for “a proper balance between preventive and curative
care, with a marked insistence on the development of healthy lifestyles.
For this purpose measures should be taken to develop individual
responsibility towards one’s own health, and ensure citizen participation
in the decision-making process concerning health care lifestyles”.

4. Budget constraints in the majority of Council of Europe member
countries weigh heavily on the public funding of health systems
as currently organised. The various budgetary contexts therefore
produce health policies based more on the treatment of disease and
on health care systems than on preventive policies.
5. The European population is undergoing demographic changes,
including population ageing, which will have serious consequences
for individuals, communities and states, alter disease patterns,
particularly as regards chronic and non-communicable diseases, and
affect the viability of health systems. Chronic conditions are projected
to be the leading cause of disability throughout the world by the
year 2020. If not successfully prevented and managed, they will
become the most expensive problems faced by our health care systems.
6. Because of growing pressure on public finances as a result
of demographic change, it is becoming vital to develop a fresh approach
that will enable every individual to enjoy the highest possible
standard of health attainable and ensure that everyone has equitable
access to it whilst maintaining budgetary balance.
7. If health policies in Europe are to be effective, therefore,
they need to incorporate an overall preventive approach so as to
be able to assimilate and address health as a state of complete
physical, mental and social well-being and not merely the absence
of disease or infirmity.
8. The rapporteur believes that investing in prevention offers
obvious economic and financial benefits. Investment in disease prevention
and health promotion can not only preserve and improve an individual’s health
and quality of life but also increase the productivity of society
and maintain a population’s work capacity. It can prevent early
death and early retirement resulting from disease, reduce business
production losses, maintain the independence of the elderly and
avoid or delay care needs.
9. At the same time, disease prevention and health promotion
enhance the population’s health competence and can thus lead to
a more highly differentiated demand for and use of health provision,
which can help to reduce the rising cost of health systems in the
long term.
10. However, inequalities in access to health education, information
and care still exist, with a well educated part of the population
who enjoy easy access to the resources allocated and disadvantaged
groups who experience greater difficulties. The real issue is therefore
how to secure access to the available resources for those most in
need.
11. An ever increasing percent of health care costs in all European
countries are attributable to chronic and preventable diseases the
kind that conventional medicine does very badly with. Our system
rewards and nurtures a therapeutic culture in which the goal is
primarily to fix what goes wrong. We have a “sickness culture” and
we need to get into a “health culture”, which must remain accessible
to the whole population.
12. This report will review existing preventive approaches to
health care and health promotion. These policies require a long-term
vision which is not completely the case yet in the Council of Europe
member states, despite existing recommendations made by several
international organisations. The rapporteur will also probe into
the costs of inaction, the advantages of prevention and the obstacles
to a genuine and comprehensive preventive health care policy. Finally
the report will discuss a number of policy pointers to take into
account when designing health promotion strategies, drawing from
the recommendations of the World Health Organization (WHO), the
conclusions of the Council of Europe European Committee of Social
Rights as well as recent public health research reports.
2. Who does
what at the international level
13. Disease prevention and health promotion have assumed
increased importance in international health policies. However,
national health policies and structures reflect deeply rooted values
and norms which differ between societies. Because of substantial
inter-country differences, it cannot be assumed that concepts are shared:
terms such as prevention, health promotion and public health are
used differently, which prevents direct comparison.
14. However, certain clear tendencies, as reflected in important
policy documents and in recommendations by European and international
organisations – in particular WHO, the Organisation for Economic
Co-operation and Development (OECD), the European Commission and
the Council of Europe – can be discerned.
15. Policy approaches are increasingly aimed at more than changing
behaviour patterns and concern themselves with health inequalities
and health determinants, that is, with the underlying causes of
health and disease. This means that other political and social fields
must be incorporated in a forward-looking health policy.
16. Although comparisons can be made between health care systems,
there is as yet no comprehensive plan for the systematic listing
and analysis of the wide range of draft laws, policies and programmes
in the fields of disease prevention and health promotion.

Here follows a brief overview of activities
of the main international organisations dealing with preventive
health care policies and health promotion actions.
2.1. World Health Organization
(WHO)
17. For many years WHO has been stressing the need for
investment in health and has published documents which are among
the most influential in the fields of disease prevention and health
promotion, such as the Ottawa Charter for Health Promotion, the
Framework Convention on Tobacco Control, the Global strategy on
Diet, Physical Activity and Health and the 2008-2013 Action plan
for the global strategy for the prevention and control of noncommunicable
diseases. As regards infectious diseases, WHO has created a global
surveillance system by setting up a “network of networks” which
combines the networks of medical laboratories and centres already
existing at the local, regional, national and international levels.
2.2. Organisation for
Economic Co-operation and Development (OECD)
18. The central theme of OECD work on health policy is
the measurement and improvement of the performance of health care
systems in member countries. Many countries possess a national framework
for measuring the performance of their health systems and have carried
out reforms. In its publication Health at a Glance 2007, the OECD
shows that health care quality, as measured by the provision of
suitable care or actual improvements in health, is making progress
in the OECD countries. However, the prevention and management of
chronic diseases pose an increasingly formidable challenge to health
policies.
2.3. European Union
(EU)
19. The EU’s health strategy focuses on health as a precondition
for economic progress, health inequalities between and within the
27 EU member states, health promotion in all policy sectors and
the mobilisation of all the parties involved. A programme of community
action in the field of public health for 2008-2013 is intended to
promote health in an ageing Europe, protect the public from threats
to health and encourage dynamic health systems and new technology.
Actions in the field of health and consumer protection are also
carried out and a European pact for mental health and well-being
helps to increase the population’s awareness of mental disorders.
2.4. Council of Europe
20. National representatives from 47 member states work
together with specialist experts to set out minimum guarantees to
safeguard human rights, the right to the protection of health and
indeed patients’ rights at the European level. Health protection
and promotion are two lines of action used to develop an ethical European
health policy. This is carried out by combining human rights, social
cohesion and health agendas, harmonising member states’ health policies
in terms of safety and quality, developing preventive medicine and health
education, and promoting patients’ rights, access to health care,
citizen participation and protection for vulnerable groups. Co-operation
activities carried out in co-operation with WHO and the European Commission,
such as the Schools for Health in Europe Network and the South-Eastern
Europe Health Network,aim
at bridging the principles and standards with real life practical
situations.
21. Preventive health care and health promotion policies certainly
benefit from transnational sharing of information and global co-operation.
However, while some overlap of activities from different organisations
is inevitable and different perspectives desirable, it would be
useful to ensure a more strategic interaction based on each organisation’s
area of specialisation. The existence of many interrelated mandates
can be confusing and redundant, especially when these must be implemented
within resource constraints that do not keep pace.
22. Efforts made by international and supranational organisations
as well as collaborative advocacy among NGOs have led to greater
recognition of the importance of health promotion policies, thus
showing a trend of policy convergence. However, there appears to
be convergence in officially stated policy but considerable divergence
in the willingness to actually implement that policy.

23. It is important to stress that health is essentially a state
responsibility and access to care remains a major concern that takes
precedence over the development of a prevention culture. While European
health systems are appreciated for their ability to make treatment
available to users at a reasonable cost, prevention policy, which
requires vision and the implementation of longer-term strategies,
does not seem to constitute a policy priority.
3. Costs of inaction
and advantages of prevention
24. At a time when budgetary pressures are having an
ever-increasing impact on how our health systems are organised,
it could be worthwhile to step up prevention policy in the hope
of making savings. One only has to take a look at the epidemiological
data to realise this.
25. Additional problems are raised by the ageing of the population.
By 2050 over a quarter of the population of the WHO European region
will be more than 65 years old. At least 35% of men over 60 suffer
from a number of chronic ailments; the number of co-morbidities
increases progressively with age and levels are higher in women.
The care of patients suffering from chronic diseases requires effective
health care services which promote health and are capable of managing
complex long-term diseases which require a patient-based approach.

26. Health indicators show a rise in chronic diseases and lifestyles
which are harmful to health. These are the symbolic diseases of
a global consumer society. Non-communicable diseases are currently
responsible for 86% of deaths and 77% of the burden of disease.
This group of conditions includes cardiovascular diseases, cancer,
mental health problems, diabetes mellitus, chronic respiratory diseases
and muscular/skeletal disorders. Cardiovascular diseases are the
chief cause of death inasmuch as they are responsible for half the deaths
in the region as a whole, with heart failure and stroke forming
the main cause of death in all countries.
27. According to WHO, seven risk factors account for nearly 60%
of the burden of disease in Europe: hypertension (12.8%), smoking
(12.3%), alcohol abuse (10.1%), raised cholesterol (8.7%), excessive
weight (7.8%), inadequate fruit and vegetable consumption (4.4%)
and lack of physical exercise (3.5%).
28. These common risk factors have economic, social, gender-linked,
political, behavioural and environmental determinants.

For
example, differences between socio-economic groups in regard to
mortality from cardiovascular diseases and risk factors giving rise
to the latter have been reported in numerous countries. Elimination
of the gap between lower and upper socio-economic groups offers
considerable scope for reducing mortality due to cardiovascular
disease and other non-communicable conditions.
29. By way of illustration, in addition to the health problems
linked to tobacco consumption, about 650 000 smoking-related deaths
occur every year in the EU. Nearly half the victims are between
35 and 69, well below average life expectancy. The direct and indirect
costs in Europe were estimated by WHO at between €97.7 and €130.3
billion in 2000, which represents between 1.04% and 1.39% of the
EU’s Gross Domestic Product (GDP).

30. People die from all chronic diseases at much lower ages in
central and eastern European countries than in Western Europe. For
example, in Hungary the cost of tobacco addiction amounted to 3.2%
of GDP in 1998, while in Finland and France the cost was estimated
at between 1.1% and 1.3% of GDP. In Sweden, the overall cost of
health care and smoking-related losses in productivity came to 26
billion Swedish kroner in 2001, which is comparable to the national
contribution to international aid (21 billion) or to the operation
of the legal system (23 billion).

31. In addition, the economic consequences of non-communicable
diseases exceed the direct cost of health services. It has been
estimated that in Sweden over 90% of total expenditure on muscular/skeletal
disorders are of an indirect nature (sick leave: 31.5%; early retirement:
59%). Premature death of the main breadwinner and of skilled workers
affects not only household income but also the national economy.
It has been estimated that the GDP of the Russian Federation was
reduced by 1% in 2005 as a result of non-communicable diseases.

32. WHO calls on countries to take measures and implement collective
action programmes aimed at the public at large, such as reduction
of the amount of salt in processed foods, reduction of the quantity
of fat in the diet, promotion of physical exercise and the consumption
of fruit and vegetables and smoking control. These actions are recognised
as the most effective ways of controlling cardiovascular diseases.
33. The first effect of prevention is to give the population as
a whole an improved quality of life by reducing the occurrence or
severity of disease and by allowing individuals to take control
over their health and well-being. Prevention also has substantial
financial effects in addition to these intangible benefits, as it
can lead to social security savings by reducing the length of time
workers are absent. A targeted prevention policy can also produce
savings in sickness insurance as such by avoiding or reducing the
cost of future treatment.
34. The competent authorities face a strong and steadily increasing
demand for an increase in the capacity of health systems to meet
the needs of consumers and patients, improve care quality and correct
disparities in health and access to care. The fact that an improvement
in general health represents an additional asset to economic growth
and therefore a further source of income is so well established
that one rarely sees it questioned. However, the rapporteur believes
that analysis of the role of power in influencing what policies
gain and lose remains currently neglected.
4. Obstacles to implementing
a genuine prevention policy
35. Data show that resources are allocated chiefly, and
at great expense, to the curative services and traditional medical
care, while primary prevention and health promotion are neglected.
On average, the OECD countries have earmarked scarcely more than
3% of their public health expenditure for a wide range of activities
such as vaccination programmes and public health campaigns against
alcohol and tobacco abuse. The great disparity largely reflects
the way prevention campaigns are organised nationally.

Proportion of public health expenditure allocated to
public health and prevention in OECD countries (2005)
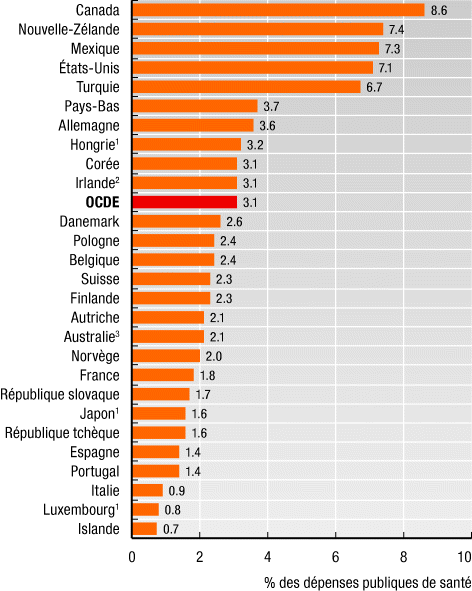
% of public health expenditure
Source: OECD Health
2007
36. It seems, moreover, that compared with the budget
for curative medicine the public authorities’ efforts regarding
disease prevention and health promotions are minimal. Public expenditure
on disease prevention in the European area represented between 0.1%
and 0.5% of GDP. By way of comparison, the Czech Republic, Iceland,
Luxembourg and Poland devoted 0.1% of GDP in the same year. The
figures were 0.2% for France, Austria, Denmark, Norway, Portugal,
the Slovak Republic, Spain, Sweden and Switzerland, 0.3% for Germany, 0.4%
for Finland, Belgium and the Netherlands and 0.5% for Hungary.

What are the reasons for this imbalance
between the funds allocated to prevention and those for the treatment
of disease?
37. A co-ordinated overall approach to prevention, a proper
continuum
based
on the participation of all parties concerned with health, education
and welfare and on the need for everyone to be aware of the importance
of health capital, encounters a number of obstacles, which are outlined
as follows:
37.1. A short-term vision:
expenditure on prevention presents a disadvantage for the competent
health authorities in that the effects of prevention efforts are
often only visible in the long term. Authorities embarking on a
large-scale prevention programme therefore run the risk of never
seeing the benefits of their policy (which are often reaped by their
successors);
37.2. Limited financial and human resources: most current health
care systems are based on responding to acute problems, urgent needs
of patients, and pressing concerns. Preventive health care is inherently
different from health care for acute problems, and in this regard,
current health care systems worldwide fall remarkably short. Prevention
budgets are always difficult to evaluate but are in any case modest.
The same applies to the staff allocated to prevention, whether they
are in school medicine, industrial medicine or public health medicine.
The training of staff not dedicated exclusively to prevention is,
furthermore, often inadequate;
37.3. The difficulty of enacting or enforcing binding rules:
this is sometimes due to the influence of powerful lobbies and economic
interests which have been able to prevent the passing of laws in
sectors such as food hygiene, agriculture, transport, industry,
tobacco and alcohol. Even when such laws exist they are often bypassed
and their application is sometimes left to the good will of the
parties involved;
37.4. The absence of genuine policy continuity and involvement
of the local authorities: prevention all too often consists of large-scale
national media campaigns without any real impact on action at the
local or field levels. Failure to assess the actions undertaken
has prevented certain innovative approaches from being pursued and
made a part of general practice;
37.5. The question of the role of the media: the information
they deliver to the general public sometimes interferes with the
perception of certain risks or of the true issues involved in disease
prevention. The close dependence between the issues on which public
opinion is focused, the policy decisions and budget allocations
often leads to a disproportion between the sums earmarked for the
reduction of certain risks and the seriousness of those risks.

38. Despite these obstacles, positive trends can be discerned,
particularly an increase in attention to strategies that concentrate
on health determinants and inequalities and focus on health gains.
Similarly, mental health is becoming more important, the introduction
of new partners is encouraging intersectoral collaboration and new
forms of organisation and financing, for example foundations, are
being tested in several countries.
39. Generally speaking, preventive actions remain all too often
based on a biomedical vision of health. Prevention can only be genuinely
effective in the health field if the living conditions available
to the population are such that it can avoid exposure to a number
of risks and is able to receive a preventive message.
5. A comprehensive
approach to preventive health care and health promotion policies:
some policy pointers
40. A country’s unique circumstances must be taken into
account when the time comes to decide on appropriate policies. National,
European and international studies and action plans on disease prevention indicate
a number of avenues to be explored or possibly useful approaches
for improving the performance of national health systems.
41. An increasing number of countries today are developing policies
and programmes that explicitly address the root causes of ill health,
health inequalities and the needs of those who are affected by poverty
and social disadvantage. This has led to a growing understanding
of the sensitivity of health to the social environment and to the
so-called social determinant of health.

Here follows a series of key actions,
policy pointers and challenges faced by policymakers:
41.1. Promoting better co-ordination
between the various policies and the so-called “health in all policies”
approach: an effective and innovative prevention policy must provide
a continuous cradle-to-grave strategy covering the preventive and
curative aspects and taking account particularly of the different
policies. Public policy can shape the social environment in ways
conducive to better health. Policies on social inclusion, education,
nutrition, agriculture, chemical production, industry, road traffic, transport,
alcohol or tobacco consumption or other fields which are not strictly
part of the health authorities’ responsibility have to be adapted
accordingly. The carrying out of health impact studies, for example
when a public policy is introduced, could assist such co-ordination
without endangering budgetary balance.
41.2. Actively co-operating with WHO and the global surveillance
system in order to halt the expansion of infectious diseases: globalisation
has brought about the rapid spread of new infectious disease, such as
SARS and HIV Aids and the re-emergence of others, such as tuberculosis
and malaria. HIV prevention, in particular, is consistently under-prioritised
in many national responses.

There
is increasing fear of global influenza pandemic and preparedness
is critical at all levels of health governance, in particular at
the international level.
41.3. Influencing risk prevention and reduction at the environmental
level (pollution, intensive use of antibiotics in livestock raising,
use of pesticides in agriculture, etc.): numerous measures aimed
at environmental hygiene are economical compared with more conventional
curative action in the health sector. To take the example of the
gradual elimination of leaded petrol, it is estimated that mental retardation
caused by exposure to lead in general is nearly 30 times higher
in regions where leaded petrol is still used than in those where
such use has ceased. The Assembly has recently examined this issue
with the Recommendation 1863 (2009) on environment and health: better
prevention of environment-related health hazards, which are referred
to for further information.

41.4. Incorporating prevention policies explicitly in poverty
reduction strategies and in relevant socio-economic policies: inequalities
in access to protection, risk exposure and access to care lead to
major inequalities in the emergence and outcome of disease. Disadvantages
tend to concentrate among the same people and their effects on health
accumulate during life. They can include having few family assets,
having a poorer education during adolescence, having insecure employment,
becoming stuck in a hazardous or dead-end job, living in poor housing,
trying to bring up a family in difficult circumstances and living
on an inadequate retirement pension. The longer people live in stressful
economic and social circumstances, the greater the physiological
wear and tear they suffer, and the less likely they are to enjoy
a healthy old age. Reducing educational failure, insecurity and
unemployment, improving housing standards, introducing minimum income
guarantees, minimum wages legislation and access to services can
help to redress the balance.
41.5. Supporting a good start in life for families and young
children: research shows that the foundations of adult health are
laid in early childhood and before birth. Slow growth and poor emotional support
raise the lifetime risk of poor physical health and reduce physical,
cognitive and emotional functioning in adulthood. Insecure emotional
attachment and poor stimulation can lead to reduced readiness for
school, low educational attainment, problem behaviour and the risk
of social marginalization in adulthood. Good health-related habits,
such as eating sensibly, exercising and not smoking, are associated
with parental and peer group examples, and with good education.
Slow or retarded physical growth in infancy is associated with reduced
cardiovascular, respiratory, pancreatic and kidney development and
function, which increase the risk of illness in adulthood. It is
critical to strengthen preventive health care before the first pregnancy
and for mothers and babies in pre- and postnatal, infant welfare
and school clinics, and through improvements in the educational
levels of parents and children.
41.6. Health education and health literacy must be a priority
of public health policy: people, children in particular, have a
right to learn about health and gain the health literacy skills
to lead a healthy lifestyle and navigate the consumer society. Health
literacy should form part of the curricula and explore the possibilities
offered by the new technologies, with a particular focus on smoking,
drugs, alcohol abuse, nutrition, mobility and safety, sport and
sex education. Participation of young people in shaping solutions to
their particular education needs is critical. Conditions at school
should also encourage the adoption of healthy behaviour through
pupils’ working, hygiene and dietary conditions. Periodical medical examinations
should be carried out throughout schooling. Immunisation programmes
should be widely accessible with high vaccination coverage rates.
Health care must be available to all children without discrimination,
including children of illegal and undocumented migrants.
41.7. Ensuring transparent decision making and accountability
in all food regulation matters, to provide affordable and nutritious
fresh food for all: a shortage of food and lack of variety cause
malnutrition and deficiency diseases. Excess intake, also a form
of malnutrition, contributes to cardiovascular diseases, diabetes,
cancer, degenerative eye diseases, obesity and dental caries. Food
poverty exists side by side with food plenty. There is confirmed
link between childhood obesity and deprivation. The important public
health issue is the availability and cost of healthy, nutritious
food. Sustainable agriculture and food production methods that conserve
natural resources and the environment should be further supported; developing
a stronger food culture for health, to foster people’s knowledge
of food and nutrition, especially aiming at children, remains critical.
41.8. Paying attention to the risks of stigmatisation: campaigns
on nutrition and healthy body weight may have unintended negative
consequences and should not stigmatise overweight people, who are likely
to deny their problem; they should also keep a watchful eye on people
at risks of developing body image and eating disorders, such as
bulimia and anorexia. Efforts should be put into identifying opportunities
for partnerships with the media and fashion industries that promote
positive body image.
41.9. Encouraging the private sector to increase its commitment
to health issues: making the industries involving potential risks
aware of their responsibilities through negotiation, fostering a
culture of corporate social responsibility; working with the food
and advertising industries to encourage the inclusion of key data,
facts and figures on non-communicable diseases and to improve the
nutrition environment, including production, supply and marketing
of food; making recommendations for reductions in levels of saturated
fat and added sugar and increased marketing of reduced/low saturated fat
and reduced/low/no sugar versions of certain food products; standards
for marketing, advertising and body image should be also explored;
advertising of harmful products should be banned.
41.10. Strengthening integration between care and prevention
by enlisting the support of health professionals: introducing health
education as a key element of initial and continuing medical training, including
in particular nutrition, health and human rights education; introducing
health literacy as a key indicator of good hospital care. This includes
a strong interest in the determinants of health and a reduction
in the routine and excessive use of medication which can be expensive,
pointless and/or harmful or even dangerous.
41.11. Promoting universal screening for risk factors at key
ages or in specific situations: facilitating family consultations
for the prevention of certain genetic or environmental risks; applying
cost-effective approaches for oral and dental disease prevention
and the early detection of breast and cervical cancer, diabetes,
hypertension and other cardiovascular risk factors. Checks and disease
testing are still sadly patchy and biased to the more affluent areas:
a universal risk assessment and management programme could significantly
increase uptake of the preventative interventions and offer a real
opportunity to reduce health inequalities.
41.12. Dealing with the wider social setting that influence use
of alcohol, drugs and tobacco: addiction is often closely associated
with markers of social and economic disadvantage; policies need
to regulate availability through pricing and licensing, to inform
people about less harmful forms of use, to use health education
to reduce recruitment of young people and to provide effective treatment
services for addicts. Trying to shift the whole responsibility on
to the user is clearly an inadequate response. This blames the victim,
rather than addressing the complexities of the social circumstances
that generate legal or illegal drug use. Effective addiction policy
must therefore be supported by the broad framework of social and economic
policy.
41.13. Adopting appropriate measures to enable elderly persons
to lead independent lives: policies should enable the elderly to
choose their life-style freely and to continue to live in their
familiar surroundings for as long as they wish and are able to,
by means of the health care and the services necessitated by their
state. In the context of a right to adequate health care for elderly
persons, Article 23 of the (revised) European Social Charter calls
for the setting-up of health care programmes and services (in particular
nursing and domiciliary care) specifically aimed at the elderly.
In addition, there should be mental health programmes for any psychological
problems in respect of the elderly and adequate palliative care
services.
41.14. Devoting special attention to mental and psychic health:
this includes the promotion of well-being, the prevention of mental
disorders, the treatment and rehabilitation of people suffering
from such disorders, and the promotion of a culture of work-life
balance; the range of suicide prevention initiatives should be extended
particularly among young people, by opting for a more comprehensive
approach to mental health in its various components (biological,
psychological and social). A national mental health policy should
also involve the social integration of highly marginalised groups
such as refugees, disaster victims, the socially excluded, the mentally
disabled, very elderly and frail people, women and children suffering
violence and the very poor.
41.15. Formulating, implementing and periodically reviewing a
coherent national policy on occupational health and safety in consultation
with employers’ and workers’ organisations: building an effective infrastructure
of workplace health protection, with legal controls and power of
inspection; promoting the right to health at work and influencing
the prevention and reduction of risks at the workplace, which is also
a suitable place from many points of view for the prevention and
early detection of non-communicable diseases; encouraging access
to sport and an active lifestyle at the workplace; promoting workplaces
which are safe, healthy and ergonomically appropriate to reduce
the burden of musculoskeletal disorders.
41.16. Developing healthy transport policies and pedestrian/cyclist-friendly
towns, in co-operation with local and regional authorities: people’s
most immediate environment is critical for their health and well-being;
better public transport translates into less driving and more walking
and cycling; increasing financial support for public transport instead
of road building; introducing the “polluter pays” principle setting
tax to the pollution caused by the use of vehicles; changing land
use, such as converting road space into green spaces, increasing
bus and cycle lanes, encouraging in-town retail trade, instead of out-of-town
supermarkets.
41.17. 41.17. Encouraging the participation of civil society
organisations: patients’ and consumers’ associations, registered
charitable bodies and non-governmental and intergovernmental organisations can
help to disseminate information and raise awareness. In addition,
participation of patients, consumers, citizens in decisions regarding
their health is a key principle of a modern public health, which encourages
co-operation, negotiation and problem-solving.
41.18. Setting-up evaluation systems for prevention policies:
it is critical to measure the evolving situation and the results
with a view to reliable monitoring of the measures taken and their
effects on the basis of indicators developed by each country; standardised
data and information collection should be promoted, encouraging
standardisation of the relevant indicators for evaluation of these
policies.

6. Conclusions
42. Prevention is primarily a way of acting and a question
of attitude as much as of means. Governments can help through certain
measures to bring about changes in representations and mentalities,
create a social, economic and environmental context that encourages
health and pave the way for a disease prevention and health promotion
culture.
43. The rapporteur believes that tomorrow’s medicine will be about
looking through a new pair of glasses which reveal the true causes
of disease. In most cases these lie in faulty nutrition, pollution,
stress, negativity, addiction and lack of exercise – the greatest
cause of all being ignorance. The original meaning of the word “doctor”
is “teacher or learned man” and that is perhaps the most important
role a health professional can perform.
44. With the 2005 Warsaw Action Plan, the Council of Europe member
states agreed that protection of health as a social human right
is an essential condition for social cohesion and economic stability.
They supported the implementation of a strategic integrated approach
to health and health-related activities. Social support is an essential
determinant of health. The chief criterion for gauging the success
of health system reform remains effective access to health care
services, including disease prevention and health promotion, for
all, without discrimination, as an individual’s fundamental right.
45. The rapporteur considers that the health sector, which is
particularly characterised by powerful pharmaceutical lobbies and
is thus subject to market laws, only seldom questions the cost/benefit
ratio of advanced techniques, which are becoming ever more expensive.
It also suffers from the lack of importance attributed to patients’
organisations, NGOs and health professionals, who could make a valuable
contribution to prevention in terms of resources and human capital.
46. International data indicate that the cost/effectiveness ratio
of health care systems can be improved.

However,
it is not sufficient to reduce costs; it is also necessary to spend
money differently and to look at health policy from an overall perspective,
incorporating an ethical, social and human rights dimension in the
reforms to be undertaken.
47. In conclusion, it seems justified to recommend concerted and
concrete action in the field of prevention by Council of Europe
member states with the aim of allocating a minimum of 0.5% of GDP
to preventive health policies.
48. It would be also desirable to further strengthen the co-operation
between the Council of Europe and WHO on health matters, inasmuch
as the Council of Europe provides a parliamentary and civil society
platform for the wider Europe.


![]() from different horizons
have pooled their experiences in the field of prevention in healthcare. Their
findings and proposals are as follows:
from different horizons
have pooled their experiences in the field of prevention in healthcare. Their
findings and proposals are as follows: